Immunity against many types of pathogens relies heavily on helper T cells, a key player that directs many downstream events of the adaptive immune response, such as aiding B cells in making antibodies, or helping macrophages phagocytose and kill bacteria. To address the role of these T cells during infection, we use mouse models combined with peptide-major histocompatibility complex class II (pMHCII) tetramers that allow us to detect and interrogate very small numbers of Salmonella-specific helper T cells throughout the course of infection. We also track antigen specific B cells allowing us to tease apart the entire adaptive immune response following vaccination, infection and disease induction.
Our lab focuses primarily on answering the following four immunological questions:
How do different infected organs affect Salmonella specific immune responses?
How can vaccines be manipulated to redirect optimal immune responses to where they are most needed?
How might mast cells control adaptive immune responses?
How do different infected organs affect Salmonella specific immune responses?
Certain bacterial infections, such as those caused by the intracellular bacteria Salmonella, are never cleared throughout the lifetime of the host once it has been infected. We want to understand why the immune system doesn’t completely clear these bacterial infections, yet prevents death caused by the pathogen. The formation of this “stalemate immunity” and the mechanisms that regulate it are some of the more interesting concepts facing immunologists studying infectious disease today. We have found that the anatomical site of Salmonella persistence leads to very different outcomes with regard to T cell and macrophage function. For example, the liver appears to induce T cells and macrophages that are more tolerant of infection whereas those from the spleen and lymph nodes are much better at bacterial clearance. Additionally, we have made the interesting observation that new T cells just “born” out of the thymus are essential for protective immunity to persistent Salmonella infection. We are now focusing on the mechanisms that regulate these organ specific responses.
throughout the lifetime of the host once it has been infected. We want to understand why the immune system doesn’t completely clear these bacterial infections, yet prevents death caused by the pathogen. The formation of this “stalemate immunity” and the mechanisms that regulate it are some of the more interesting concepts facing immunologists studying infectious disease today. We have found that the anatomical site of Salmonella persistence leads to very different outcomes with regard to T cell and macrophage function. For example, the liver appears to induce T cells and macrophages that are more tolerant of infection whereas those from the spleen and lymph nodes are much better at bacterial clearance. Additionally, we have made the interesting observation that new T cells just “born” out of the thymus are essential for protective immunity to persistent Salmonella infection. We are now focusing on the mechanisms that regulate these organ specific responses.
How can vaccines be manipulated to redirect optimal immune responses to where they are most needed?
Attempting to understand bacterial immunity also informs another focus of the lab: defining mechanisms of vaccine-mediated immunity, particularly against enteric pathogens like Salmonella. For pathogens such as this, it would be desirable to direct immune cells to the intestines where they can target the bacteria at their initial  entry point, but it is unclear how this might be achieved. While it is known that vaccines given via traditional routes, i.e. intramuscularly, can protect against many infectious diseases, it is less clear how changing routes or vaccine make-up can affect immune cell migration or phenotype. Does immunizing in skin direct a different response compared to immunizing via another route? Does the type of adjuvant change the predominant immune response from antibody-dominated to one that is more cell-mediated? We are investigating these questions using different types of vaccine adjuvants and immunization routes combined with pMHCII tetramers. Our ultimate goal is to be able to imprint an anatomical “zip code” for the correct type of cells against a particular pathogen based purely on vaccine design.
entry point, but it is unclear how this might be achieved. While it is known that vaccines given via traditional routes, i.e. intramuscularly, can protect against many infectious diseases, it is less clear how changing routes or vaccine make-up can affect immune cell migration or phenotype. Does immunizing in skin direct a different response compared to immunizing via another route? Does the type of adjuvant change the predominant immune response from antibody-dominated to one that is more cell-mediated? We are investigating these questions using different types of vaccine adjuvants and immunization routes combined with pMHCII tetramers. Our ultimate goal is to be able to imprint an anatomical “zip code” for the correct type of cells against a particular pathogen based purely on vaccine design.
How might mast cells control adaptive immune responses?
Mast cells were originally characterized more than 130 years ago and were described as tissue-resident cells at the host-environment interface or localized around blood vessels. Notably, these cells have unusual cytoplasmic granules now known to contain a multitude of physiologically active compounds, including proteases, histamine,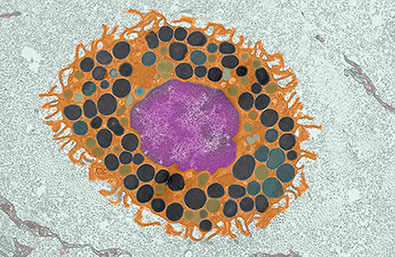 heparin and multiple cytokines. These compounds can be released upon stimulation, predominantly with the antibody IgE. This is the basis for most allergy and asthma and it is well-known that mast cells are the major contributor to these diseases. What is less appreciated is how mast cells might contribute to antibacterial immunity, especially with respect to activating the adaptive immune response against pathogens. We are addressing this by activating mast cells using various conditions and determining how downstream immune responses behave, particularly with respect to pathogen-specific T cell responses. We believe that a better understanding of how mast cells initiate and contribute to adaptive immunity will not only answer basic biological questions about how cells communicate within the immune system; it may provide opportunities to target mast cells as cellular adjuvants to target cellular immune responses specific for certain pathogens or pathogen classes.
heparin and multiple cytokines. These compounds can be released upon stimulation, predominantly with the antibody IgE. This is the basis for most allergy and asthma and it is well-known that mast cells are the major contributor to these diseases. What is less appreciated is how mast cells might contribute to antibacterial immunity, especially with respect to activating the adaptive immune response against pathogens. We are addressing this by activating mast cells using various conditions and determining how downstream immune responses behave, particularly with respect to pathogen-specific T cell responses. We believe that a better understanding of how mast cells initiate and contribute to adaptive immunity will not only answer basic biological questions about how cells communicate within the immune system; it may provide opportunities to target mast cells as cellular adjuvants to target cellular immune responses specific for certain pathogens or pathogen classes.
Why do men and women differ immunologically and how can this be exploited to develop better vaccines?
One of the great questions in biology is why men and women differ in how they respond immunologically to various insults. It is known that women respond better to vaccines and many infections, yet this increased  immune response often manifests in increased susceptibility to autoimmune disease in women compared to men. In fact, women are three times more likely to be diagnosed with multiple sclerosis and nine times more likely to have lupus when compared to men of a similar age. We are interested in understanding the mechanisms that dictate these differences. Using mouse models, we are exploring how males and females respond to infection, vaccination, and autoimmune disease induction. We are particularly interested in defining how T cell and B cells might behave differently in different tissues and whether the differences we see are cell intrinsic (programmed into the cell when it develops) or cell extrinsic (changes depending on the surrounding environment). Revealing how these disparities are established could lead to potential therapies for autoimmune diseases or help in designing more effective vaccines depending on the sex of the person receiving the immunization.
immune response often manifests in increased susceptibility to autoimmune disease in women compared to men. In fact, women are three times more likely to be diagnosed with multiple sclerosis and nine times more likely to have lupus when compared to men of a similar age. We are interested in understanding the mechanisms that dictate these differences. Using mouse models, we are exploring how males and females respond to infection, vaccination, and autoimmune disease induction. We are particularly interested in defining how T cell and B cells might behave differently in different tissues and whether the differences we see are cell intrinsic (programmed into the cell when it develops) or cell extrinsic (changes depending on the surrounding environment). Revealing how these disparities are established could lead to potential therapies for autoimmune diseases or help in designing more effective vaccines depending on the sex of the person receiving the immunization.
Copyright ©McLachlan Lab 2020
Twitter: @McLachlanLab
